Zehna Therapeutics is developing non-bactericidal inhibitors of selected gut microbial enzymes clinically and mechanistically linked with cardiometabolic diseases. Our lead compounds inhibit the gut microbial enzyme CutC lyase, preventing the conversion of dietary choline to trimethylamine (TMA) and subsequently to trimethylamine N-oxide (TMAO) within the host.
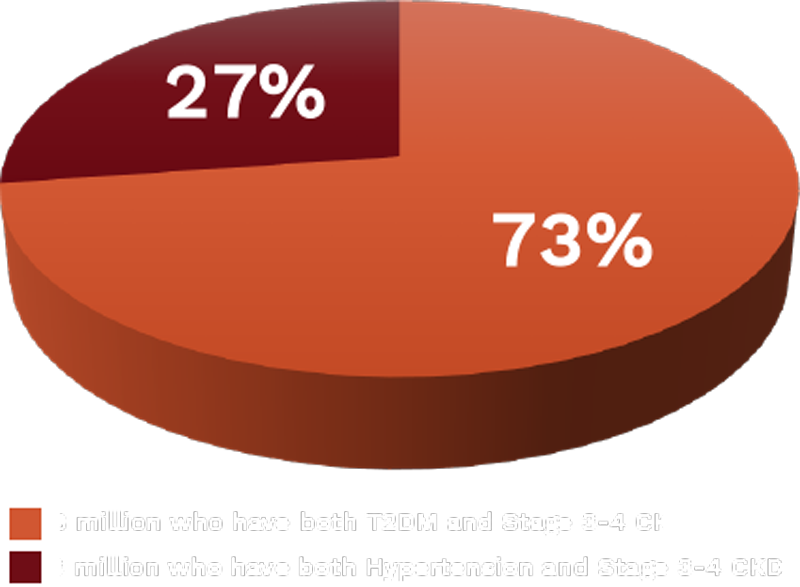
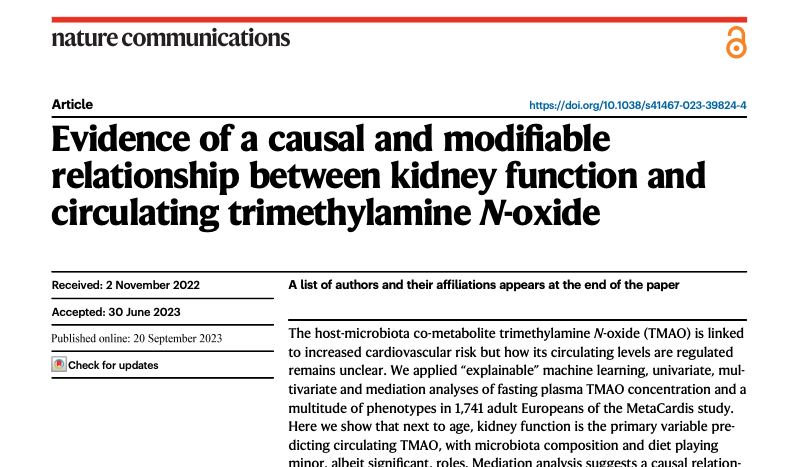
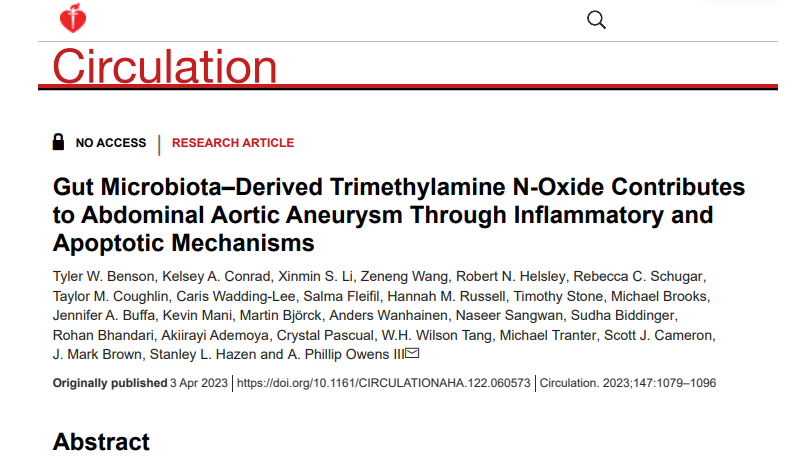
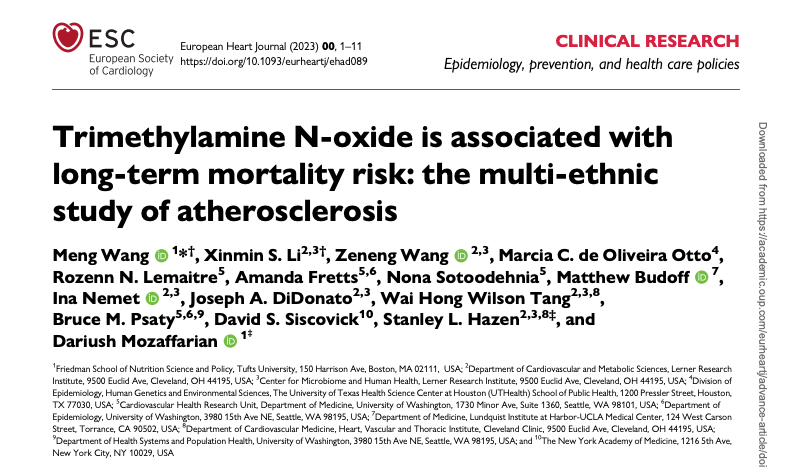
High systemic levels of TMAO have been linked to accelerated development of both cardiovascular and chronic kidney disease, as demonstrated in large-scale clinical cohort studies and extensive animal models of chronic metabolic diseases. Additionally, elevated TMAO, which often accompanies obesity, may contribute to sustained weight gain and promote renal oxidative stress and inflammation underlying obesity-associated chronic kidney disease (CKD). CKD is our lead indication.