Zehna Therapeutics is developing non-bacteriocidal inhibitors of selected gut microbial pathways clinically and mechanistically linked with chronic metabolic diseases. Our lead compounds inhibit the gut microbial enzyme CutC, preventing the conversion of dietary choline to trimethylamine (TMA) and subsequently to trimethylamine N-oxide (TMAO) within the host. High systemic levels of TMAO have been linked to accelerated development of both cardiovascular and chronic kidney disease, as demonstrated in large-scale clinical cohort studies. Chronic Kidney Disease is our lead indication.
First-in-Class
CutC Inhibitor
Our science starts with the microbiome
- Bacteria in the gut possess an enzyme, CutC, that converts dietary choline into TMA
- TMA is absorbed and transformed by human liver enzymes into TMAO, which is associated with deleterious kidney effects
- At Zehna, we are designing small molecules to inhibit CutC and prevent the formation of TMA and TMAO, with the aim of slowing chronic kidney disease progression
What makes our approach different
- We are targeting a driver of disease, rather than a symptom
- Unlike the standard of care interventions, we are drugging the microbiome, not the human host
- We employ well-established drug discovery principles to inhibit a bacterial enzyme target with a small molecule
1 (Evenepoel 2017)
2 (Kanbay 2018)
3 (Sumida 2019; Mahmoodpoor 2017; Sampaio-Maia 2016)
4 (Lin 2017; Vaziri 2013)
5 (Tang 2015; Rhee 2013; Gruppen 2017; Zhang 2021)
6 (Loo 2021; Zeisel 2017)
7 (Dolphin 1997; Bennet 2013; Schmidt 2020; Gatarek 2021)
8 (Stubbs 2016; Missailidis 2016; Kim 2016; Zhou 2021; Tang 2015; Gupta 2020; Fang 2021; Lai 2021; Kapetanaki 2021; Zhang 2021)
9 (Roberts 2018; Gupta 2020; Gatarek 2021)
Chronic Kidney Disease (CKD)
CKD is Common, Serious and Costly
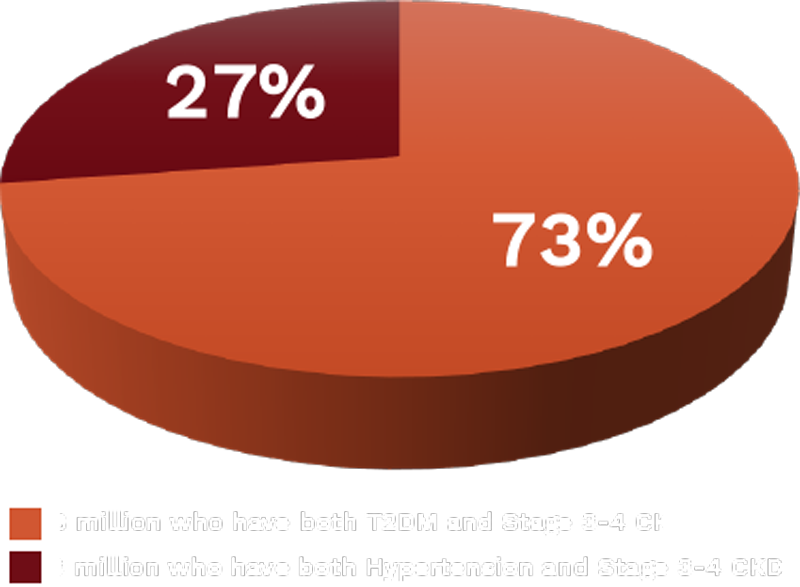
CKD is prevalent in individuals with type 2 diabetes mellitus (T2DM) and hypertension:
- >33 million people in U.S with T2DM2; 24.5% or 8 million have both T2DM and stage 3 – 4 CKD2
- ~50% people in U.S. with hypertension1; 24% have their hypertension under control1; ~3 million people with both hypertension and stage 3 – 4 CKD
- $20.96B global sales forecast in CKD market by 20283
1 Kovesdy Kidney International, 2022
2 CDC.gov
3 Data Bridge

11 Million People with Stage 3-4 CKD
Timeline of Discoveries Establishing TMAO as a Driver of CKD
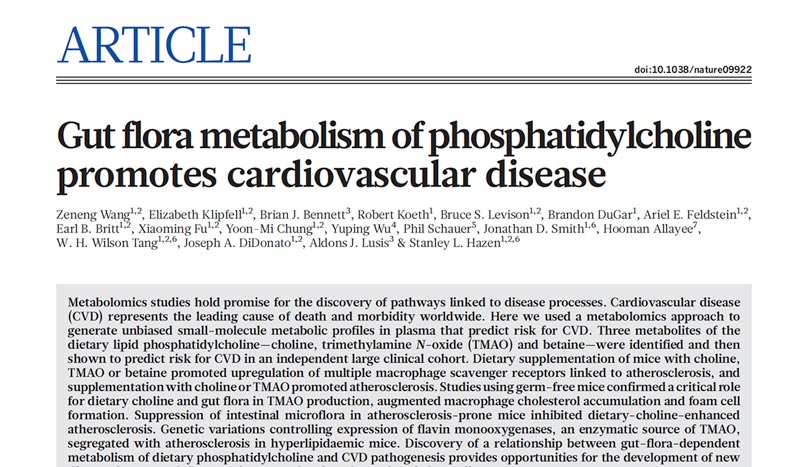
- Wang Z, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature. 2011; 472:57 – 63.
- Tang WH, Wang Z, Levison BS, et al. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med. 2013 Apr 25;368(17):1575-84.
- Rhee EP, Clish CB, Ghorbani A, et al. A combined epidemiologic and metabolomic approach improves CKD prediction. J Am Soc Nephrol. 2013 Jul;24(8):1330-8.
- Tang WH, Wang Z, Kennedy DJ, et al. Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ Res. 2015;116(3):448-455.
- Stubbs JR, House JA, Ocque AJ, et al. Serum trimethylamine-N-oxide is elevated in CKD and correlates with coronary atherosclerosis burden. J Am Soc Nephrol. 2016;27(1):305-313.
- Kim RB, Morse BL, Djurdjev O, et al.; CanPREDDICT Investigators. Advanced chronic kidney disease populations have elevated trimethylamine N-oxide levels associated with increased cardiovascular events. Kidney Int. 2016;89(5):1144-1152.
- Missailidis C, Hällqvist J, Qureshi AR, et al. Serum trimethylamine-N-oxide is strongly related to renal function and predicts outcome in chronic kidney disease. PLoS One. 2016;11(1):e0141738.
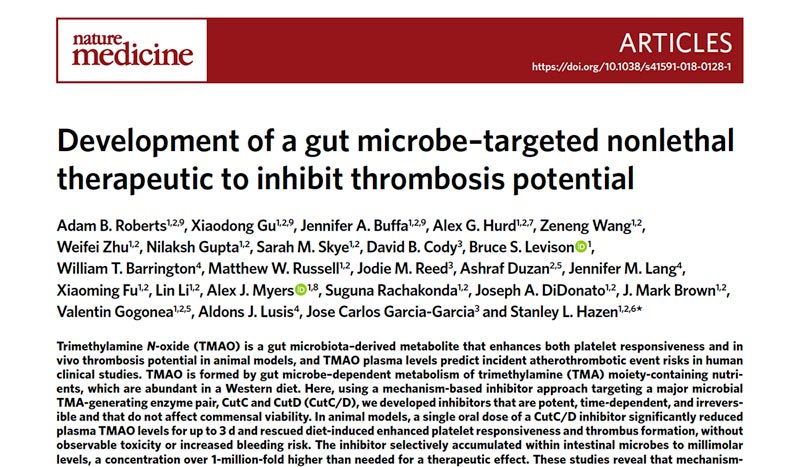
- Roberts AB, Gu X, Buffa JA, et al. Development of a gut microbe-targeted nonlethal therapeutic to inhibit thrombosis potential. Nat Med. 2018;24(9):1407-1417.
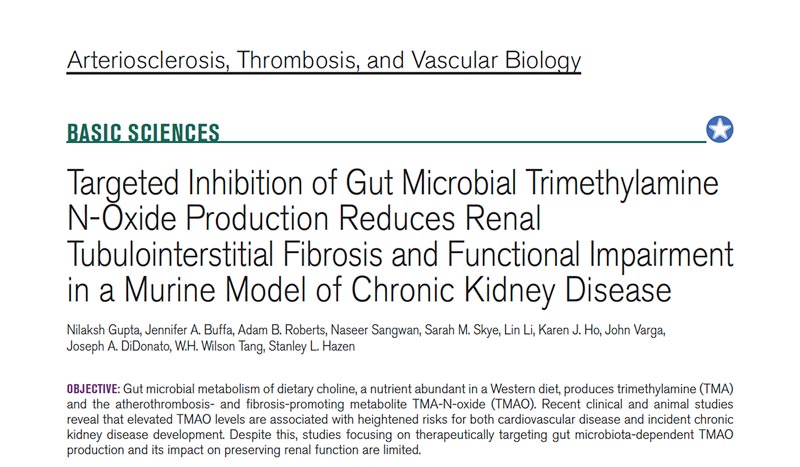
- Gupta N, Buffa JA, Roberts AB, et al. Targeted inhibition of gut microbial trimethylamine n-oxide production reduces renal tubulointerstitial fibrosis and functional impairment in a murine model of chronic kidney disease. Arterioscler Thromb Vasc Biol. 2020;40(5):1239-1255.
- Zeng Y, Guo M, Fang X, et al. Gut microbiota-derived trimethylamine N-oxide and kidney function: a systemic review and meta-analysis. Adv. Nutr. 2021;12:1286 – 1304.
- Zhou J, Wang, D, Li B, et al. Relationship between plasma trimethylamine N-oxide levels and renal dysfunction in patients with hypertension. Kidney Blood Press Res. 2021;46:421-432.
PUBLICATIONS
Targeted Inhibition of Gut Microbial Trimethylamine N-Oxide Production Reduces Renal Tubulo…
Basic Sciences
May 2020
Development Of A Gut Microbe–Targeted Nonlethal Therapeutic To Inhibit Thrombosis Potential
Nature Medicine
September 2018
Evidence that TMAO Pathway Drives CKD in Humans
Study
Observations
Rhee et al. J Am Soc Nephrol. 2013
The Framingham Heart Study identified elevated TMAO in a non-CKD cohort as an increased risk factor for incident CKD
Stubbs et al. J Am Soc Nephrol. 2016
Serum TMAO is inversely correlated with eGFR and is an independent risk factor for coronary atherosclerosis burden and mortality in CKD patients
Missailidis et al. PLoS One. 2016
Elevated TMAO is associated with increased inflammation and increased risk for all-cause mortality in CKD patients
Kim et al. Kidney Int. 2016
High baseline TMAO (>20 mM) is independently associated with CV events
Zhou et al. Kidney Blood Press Res. 2021
Elevated TMAO is associated with severe renal dysfunction and is predictive of early kidney disease in hypertensive patients
Tang et al. Circ Res. 2015
TMAO levels were markedly higher in CKD vs non-CKD patients; within CKD, TMAO in the highest quartile was independently associated with an increased mortality risk